Originally posted on UCLA Newsroom
Acollaboration led by UCLA and the Seattle Children’s Research Institute has yielded new knowledge about the genes responsible for the production and release of immunoglobulin G, the most common type of antibody in the human body.
The finding has the potential to advance manufacturing of antibody-based therapies for diseases such as cancer and arthritis, as well as the development of medical treatments that rely on the production of antibodies.
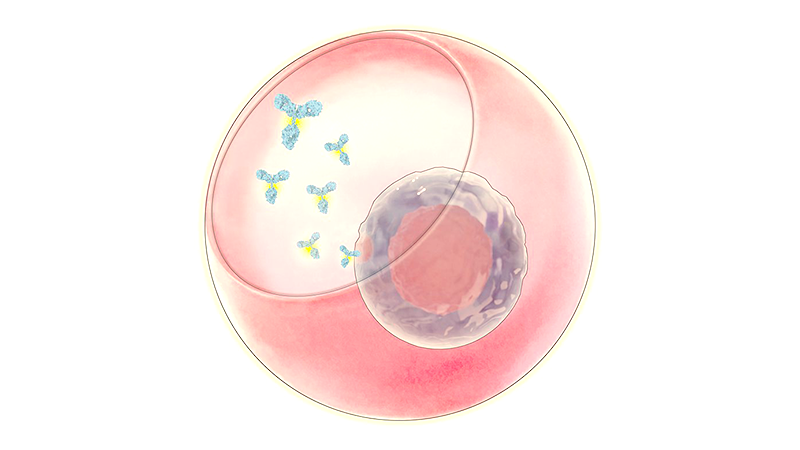
Antibodies are a group of proteins that are crucial to the immune system. Immunoglobulin G, or IgG, stores memories of past infections and tags dangerous microbes to be eliminated by immune cells. Mothers’ IgG is also vital for their newborns’ immune defense.
Scientists have known for decades that a population of white blood cells, called plasma B cells, make IgG. Plasma B cells are highly efficient, producing more than 10,000 IgG molecules every second. But the molecular mechanisms that enable plasma cells to secrete antibodies into the bloodstream are still not fully understood.
In order to learn more about those mechanisms, the researchers performed an analysis that had never been done before: They captured thousands of single plasma B cells as well as their individual secretions, and then connected the amount of proteins each individual cell released to an atlas mapping tens of thousands of genes expressed by that same cell.
To collect the cells and their secretions, the researchers used microscopic, bowl-shaped hydrogel containers called nanovials, which were developed in prior UCLA research.
Their analysis found that genes involved with producing energy and eliminating abnormal proteins were even more important for high IgG secretion than the genes containing instructions for making the antibody itself. They also discovered that the presence of CD59, a gene that had not previously been linked to IgG secretion, is a better predictor of high-producing plasma cells than other genetic markers already associated with this cell type.
“These processes in cells are like an assembly line for making proteins, and there are lots of places where you could see bottlenecks,” said Dino Di Carlo, the Armond and Elena Hairapetian Professor of Engineering and Medicine at the UCLA Samueli School of Engineering and a co-corresponding author of the study. “Things have to be moving smoothly in sync across the cell. If a cell is making a lot of proteins, it’s using a lot of energy and needs a way to correct the proteins that get messed up.”
The study was published in the journal Nature Communications. Di Carlo, who is also a member of the California NanoSystems Institute at UCLA and the UCLA Jonsson Comprehensive Cancer Center, said the findings could not only advance fundamental understandings of biology but also could have applications in biomedicine.
For instance, knowing which genes are associated with higher secretion of an antibody could be used by pharmaceutical makers to engineer cells that secrete large volumes of the antibody. That knowledge could also be applied to an emerging strategy that introduces engineered cells directly to patients’ bodies, such as the potential cell therapies under development by University of Washington immunologist Richard James, a co-corresponding author of the paper.
The new way in which nanovials and a standard laboratory setup were used in the study also opens up new possibilities for understanding how the instructions contained in DNA are translated into the behaviors of cells.
Each nanovial contains molecules tailored to bind with proteins on the surface of the cells that the researchers are investigating, which enables the nanovial to capture a single cell at a time. Once that cell is immobilized and protected within the nanovial “bowl,” its secretions also accumulate and are attached to specific antibodies engineered to capture them.
In the study, the investigators trapped tens of thousands of plasma cells, along with the IgG they released, in nanovials with a diameter about one-third the thickness of a sheet of paper. The nanovials were then run through an instrument to analyze each cell’s messenger RNA, or mRNA.
Every cell in an individual’s body carries the same blueprint written in DNA. So scientists detect which genes are active by looking at the mRNA, which translates those instructions so that each cell can build proteins that are specific to its functions.
“There are multiple layers of information in each cell,” Di Carlo said. “We’re able to link the final layer — the amount of proteins actually secreted that have a clear function throughout the body — back to the more fundamental layer of genetic code. There’s currently no other technique that is available to do that. Now that we have this approach, the most interesting thing, to me, is which question to ask next.”
In future studies, the researchers hope to identify all of the genes that affect plasma cells’ production and secretion of IgG.
Nanovials are available commercially from Partillion Bioscience, a company co-founded by Di Carlo that is based in CNSI’s on-campus startup incubator, Magnify.
The first authors of the study are Rene Cheng of the University of Washington and Joseph de Rutte, who earned a doctorate from UCLA in 2020 and is a co-founder and CEO of Partillion. Other authors are affiliated with UW, Partillion and the Seattle-based company Luminex. The study was supported by the National Institutes of Health and the Seattle Children’s Research Institute.